Humans and vertebrates have a single structural plan and are represented by the central part - the brain and spinal cord, as well as the peripheral section - nerves extending from the central organs, which are processes of nerve cells - neurons.
Features of neuroglial cells
As we have already said, the myelin sheath of dendrites and axons is formed by special structures characterized by a low degree of permeability for sodium and calcium ions, and therefore having only resting potentials (they cannot conduct nerve impulses and perform electrical insulating functions).
These structures are called These include:
- oligodendrocytes;
- fibrous astrocytes;
- ependyma cells;
- plasma astrocytes.
All of them are formed from the outer layer of the embryo - the ectoderm and have a common name - macroglia. The glia of the sympathetic, parasympathetic and somatic nerves are represented by Schwann cells (neurolemmocytes).
The structure and functions of oligodendrocytes
They are part of the central nervous system and are macroglial cells. Since myelin is a protein-lipid structure, it helps to increase the speed of excitation. The cells themselves form an electrically insulating layer of nerve endings in the brain and spinal cord, forming already in the period of intrauterine development. Their processes wrap neurons, as well as dendrites and axons, in the folds of their outer plasmalemma. It turns out that myelin is the main electrically insulating material that delimits the nerve processes of mixed nerves.

and their features
The myelin sheath of the nerves of the peripheral system is formed by neurolemmocytes (Schwann cells). Their distinguishing feature is that they are able to form a protective sheath of only one axon, and cannot form processes, as is inherent in oligodendrocytes.
Between the Schwann cells at a distance of 1-2 mm there are areas devoid of myelin, the so-called nodes of Ranvier. Through them, electrical impulses are carried out spasmodically within the axon.
Lemmocytes are capable of repairing nerve fibers, and also perform. As a result of genetic aberrations, the cells of the membrane of lemmocytes begin uncontrolled mitotic division and growth, as a result of which tumors - schwannomas (neurinomas) develop in various parts of the nervous system.
The role of microglia in the destruction of the myelin structure
Microglia are macrophages capable of phagocytosis and able to recognize various pathogenic particles - antigens. Thanks to membrane receptors, these glial cells produce enzymes - proteases, as well as cytokines, for example, interleukin 1. It is a mediator of the inflammatory process and immunity.
The myelin sheath, whose function is to isolate the axial cylinder and improve the conduction of the nerve impulse, can be damaged by interleukin. As a result, the nerve is "bare" and the rate of excitation is sharply reduced.

Moreover, cytokines, by activating receptors, provoke excessive transport of calcium ions into the body of the neuron. Proteases and phospholipases begin to break down the organelles and processes of nerve cells, which leads to apoptosis - the death of this structure.
It collapses, disintegrating into particles, which are devoured by macrophages. This phenomenon is called excitotoxicity. It causes degeneration of neurons and their endings, leading to diseases such as Alzheimer's disease and Parkinson's disease.
Pulp nerve fibers
If the processes of neurons - dendrites and axons, are covered with a myelin sheath, then they are called pulpy and innervate the skeletal muscles, entering the somatic section of the peripheral nervous system. Unmyelinated fibers form the autonomic nervous system and innervate internal organs.

The pulpy processes have a larger diameter than the non-fleshy ones and are formed as follows: axons bend the plasma membrane of glial cells and form linear mesaxons. Then they elongate and the Schwann cells repeatedly wrap around the axon, forming concentric layers. The cytoplasm and nucleus of the lemmocyte move to the region of the outer layer, which is called the neurilemma or the Schwann membrane.
The inner layer of the lemmocyte consists of a layered mesoxon and is called the myelin sheath. Its thickness in different parts of the nerve is not the same.
How to repair myelin sheath
Considering the role of microglia in the process of nerve demyelination, we found that under the action of macrophages and neurotransmitters (for example, interleukins) myelin is destroyed, which in turn leads to a deterioration in the nutrition of neurons and a disruption in the transmission of nerve impulses along axons.
This pathology provokes the occurrence of neurodegenerative phenomena: deterioration of cognitive processes, primarily memory and thinking, the appearance of impaired coordination of body movements and fine motor skills.

As a result, complete disability of the patient is possible, which occurs as a result of autoimmune diseases. Therefore, the question of how to restore myelin is currently particularly acute. These methods include primarily a balanced protein-lipid diet, proper lifestyle, and the absence of bad habits. In severe cases of diseases, drug treatment is used to restore the number of mature glial cells - oligodendrocytes.
The nervous system of humans and vertebrates has a single structural plan and is represented by the central part - the brain and spinal cord, as well as the peripheral section - depart from the central organs by nerves, which are processes of nerve cells - neurons.
Their combination forms the nervous tissue, the main functions of which are excitability and conductivity. These properties are explained primarily by the structural features of the shells of neurons and their processes, consisting of a substance called myelin. In this article, we will consider the structure and functions of this compound, as well as find out possible ways to restore it.
Why are neurocytes and their processes covered with myelin
It is no coincidence that dendrites and axons have a protective layer consisting of protein-lipid complexes. The fact is that the violation is a biophysical process, which is based on weak electrical impulses. If electric current flows through the wire, then the latter must be covered with insulating material in order to reduce the dispersion of electrical impulses and prevent a decrease in current strength. The myelin sheath performs the same functions in the nerve fiber. In addition, it is a support and also provides power to the fiber.
The chemical composition of myelin
Like most cell membranes, it has a lipoprotein nature. Moreover, the fat content here is very high - up to 75%, and proteins - up to 25%. Myelin also contains a small amount of glycolipids and glycoproteins. Its chemical composition differs in the spinal and cranial nerves.
In the former, there is a high content of phospholipids - up to 45%, and the rest falls on cholesterol and cerebrosides. Demyelination (that is, the replacement of myelin with other substances in the nerve processes) leads to such severe autoimmune diseases as, for example, multiple sclerosis.
From a chemical point of view, this process will look like this: the myelin sheath of nerve fibers changes its structure, which is manifested primarily in a decrease in the percentage of lipids relative to proteins. Further, the amount of cholesterol decreases and the water content increases. And all this leads to a gradual replacement of myelin, which contains oligodendrocytes or Schwann cells, macrophages, astrocytes and intercellular fluid. The result of such biochemical changes will be a sharp decrease in the ability of axons to conduct excitation up to the complete blocking of the passage of nerve impulses.
Features of neuroglial cells
As we have already said, the myelin sheath of dendrites and axons is formed by special structures that are characterized by a low degree of permeability for sodium and calcium ions, and therefore have only resting potentials (they cannot conduct nerve impulses and perform electrical insulating functions). These structures are called glial cells. These include:
- oligodendrocytes;
- fibrous astrocytes;
- ependymal cells;
- plasma astrocytes.
All of them are formed from the outer layer of the embryo - the ectoderm and have a common name - macroglia. The glia of the sympathetic and parasympathetic somatic nerves are represented by Schwann cells (neurolemmocytes).
The structure and functions of oligodendrocytes
They are part of the central nervous system and are macroglial cells. Since myelin is a protein-lipid structure, it helps to increase the speed of excitation. The cells themselves form an electrically insulating layer of nerve endings in the brain and spinal cord, forming already in the period of intrauterine development. Their processes wrap neurons, as well as dendrites and axons, in the folds of their outer plasmalemma. It turns out that myelin is the main electrically insulating material that delimits the nerve processes of mixed nerves.
Schwann cells and their features
The myelin sheath of the nerves of the peripheral system is formed by neurolemmocytes (Schwann cells). Their distinguishing feature is that they are able to form a protective sheath of only one axon, and cannot form processes, as is inherent in oligodendrocytes. Between the Schwann cells at a distance of 1-2 mm there are areas devoid of myelin, the so-called nodes of Ranvier. Behind it, electrical impulses are carried out spasmodically within the axon. Lemmocytes are capable of repairing nerve fibers, and also perform a trophic function. As a result of genetic aberrations, lemmocyte envelope cells begin uncontrolled mitotic division and growth, as a result of which tumors, schwannomas (neurinomas), develop in different parts of the nervous system.
The role of microglia in the destruction of the myelin structure
Microglia are macrophages capable of phagocytosis and are able to recognize various pathogenic particles - antigens. Thanks to membrane receptors, these glial cells produce enzymes - proteases, as well as cytokines, for example, interleukin 1. It is a mediator of the inflammatory process and immunity. The myelin sheath, whose function is to isolate the axial cylinder and improve nerve impulse conduction, can be damaged by interleukin. As a result, the nerve is “exposed” and the rate of excitation conduction is sharply reduced.
Moreover, cytokines, by activating receptors, provoke excessive transport of calcium ions into the body of the neuron. Proteases and phospholipases begin to break down the organelles and processes of nerve cells, which leads to apoptosis - the death of this structure. It collapses, disintegrating into particles, which are devoured by macrophages. This phenomenon is called excitotoxicity. It causes degeneration of neurons and their endings, leading to diseases such as Alzheimer's disease and Parkinson's disease.
Pulp nerve fibers
If the processes of neurons - dendrites and axons, are covered with a myelin sheath, then they are called pulpy and innervate the skeletal muscles, entering the somatic section of the peripheral nervous system. Unmyelinated fibers form the autonomic nervous system and innervate internal organs.
The pulpy processes have a larger diameter than the non-pulmonic processes and are formed as follows: axons bend the plasma membrane of glial cells and form linear mesaxons. They then enlarge and the Schwann cells repeatedly wrap around the axon, forming concentric layers. The cytoplasm and nucleus of the lemmocyte move to the region of the outer layer, which is called the neurilemma or the Schwann membrane. The inner layer of the lemmocyte consists of a layered mesoxon and is called the myelin sheath. Its thickness in different parts of the nerve is not the same.
How to repair myelin sheath
Considering the role of microglia in the process of nerve demyelination, we found that under the action of macrophages and neurotransmitters (for example, interleukins) myelin is destroyed, which in turn leads to a deterioration in the nutrition of neurons and a violation of the transmission of nerve impulses along axons. This pathology provokes the occurrence of neurodegenerative phenomena: deterioration of cognitive processes, primarily memory and thinking, the appearance of impaired coordination of body movements and fine motor skills.
As a result, complete disability of the patient is possible, which occurs as a result of autoimmune diseases. Therefore, the question of how to restore myelin is currently particularly acute. These methods include, first of all, a balanced protein-lipid diet, proper lifestyle, and the absence of bad habits. In severe cases of diseases, drug treatment is used to restore the number of mature glial cells - oligodendrocytes.
Publication date: 05/26/17The central nervous system (CNS) is a single mechanism that is responsible for the perception of the surrounding world and reflexes, as well as for controlling the system of internal organs and tissues. The last point is performed by the peripheral part of the central nervous system with the help of special cells called neurons. Nervous tissue consists of them, which serves to transmit impulses.
The processes coming from the body of the neuron are surrounded by a protective layer that nourishes the nerve fibers and accelerates the transmission of impulses, and such protection is called the myelin sheath. Any signal transmitted through the nerve fibers resembles a discharge of current, and it is their outer layer that does not allow its strength to decrease.
If the myelin sheath is damaged, then full perception in this part of the body is lost, but the cell can survive and the damage heals over time. With sufficiently serious injuries, drugs designed to restore nerve fibers like Milgamma, Copaxone and others will be required. Otherwise, the nerve will eventually die and perception will decrease. The diseases that are characterized by this problem include radiculopathy, polyneuropathy, etc., but doctors consider multiple sclerosis (MS) to be the most dangerous pathological process. Despite the strange name, the disease has nothing to do with the direct definition of these words and means "multiple scars" in translation. They occur on the myelin sheath in the spinal cord and brain due to immune failure, so MS is an autoimmune disease. Instead of nerve fibers, a scar appears at the site of the focus, consisting of connective tissue, through which the impulse can no longer pass correctly.
Is it possible to somehow restore the damaged nervous tissue or will it forever remain in a crippled state? Doctors still cannot answer it accurately and have not yet come up with a full-fledged drug to restore sensitivity to nerve endings. Instead, there are various medications that can reduce the demyelination process, improve the nutrition of damaged areas and activate the regeneration of the myelin sheath.
Milgamma is a neuroprotector for restoring metabolism inside cells, which allows you to slow down the process of myelin destruction and start its regeneration. The drug is based on vitamins from group B, namely:
- Thiamine (B1). It is essential for the absorption of sugar in the body and energy. With acute thiamine deficiency in a person, sleep is disturbed and memory deteriorates. He becomes nervous and sometimes depressed, as in depression. In some cases, there are symptoms of paresthesia (goosebumps, decreased sensitivity and tingling in the fingertips);
- Pyridoxine (B6). This vitamin plays an important role in the production of amino acids, as well as some hormones (dopamine, serotonin, etc.). Despite rare cases of lack of pyridoxine in the body, due to its deficiency, a decrease in mental abilities and a weakening of immune defenses are possible;
- Cyanocobalamin (B12). It serves to improve the conductivity of nerve fibers, resulting in improved sensitivity, as well as to improve blood synthesis. With a lack of cyanocobalamin, a person develops hallucinations, dementia (dementia), there are disruptions in the heart rhythm and paresthesia.
Thanks to this composition, Milgama is able to stop the oxidation of cells by free radicals (reactive substances), which will affect the restoration of the sensitivity of tissues and nerve endings. After a course of taking the tablets, there is a decrease in symptoms and an improvement in the general condition, and the drug should be taken in 2 stages. In the first, you will need to make at least 10 injections, and then switch to tablets (Milgamma compositum) and take them 3 times a day for 1.5 months.

Stafaglabrin sulfate has been used for a long time to restore the sensitivity of tissues and the nerve fibers themselves. The plant from whose roots this drug is extracted grows only in subtropical and tropical climates, for example, in Japan, India and Burma, and it is called Stephania smooth. There are cases of obtaining Stafaglabrin sulfate in the laboratory. Perhaps this is due to the fact that stephania smooth can be grown as a suspension culture, that is, in a suspended position in glass flasks with liquid. By itself, the drug is a sulfate salt, which has a high melting point (more than 240 ° C). It refers to the alkaloid (nitrogen-containing compound) stefarine, which is considered the basis for proaporphin.
Stefaglabrin sulfate serves to reduce the activity of enzymes from the class of hydrolases (cholinesterase) and to improve the tone of smooth muscles that are present in the walls of blood vessels, organs (hollow inside) and lymph nodes. It is also known that the drug is slightly toxic and can reduce blood pressure. In the old days, the drug was used as an anticholinesterase agent, but then scientists came to the conclusion that Stefaglabrin sulfate is an inhibitor of connective tissue growth activity. From this it turns out that it delays its development and scars do not form on the nerve fibers. That is why the drug began to be actively used for damage to the PNS.
During the research, experts were able to see the growth of Schwann cells, which produce myelin in the peripheral nervous system. This phenomenon means that under the influence of the drug, the patient noticeably improves the conduction of the impulse along the axon, since the myelin sheath again began to form around it. Since the results were obtained, the drug has become a hope for many people diagnosed with incurable demyelinating pathologies.

It will not be possible to solve the problem of autoimmune pathology only by restoring nerve fibers. Indeed, no matter how many foci of damage have to be eliminated, the problem will return, since the immune system reacts to myelin as a foreign body and destroys it. To date, it is impossible to eliminate such a pathological process, but one can no longer wonder whether the nerve fibers are restored or not. People are left to maintain their condition by suppressing the immune system and using drugs like Stefaglabrin sulfate to maintain their health.
The drug can only be used parenterally, that is, by the intestines, for example, by injection. The dosage in this case should not exceed 7-8 ml of a 0.25% solution per day for 2 injections. Judging by time, the myelin sheath and nerve endings are usually restored to some extent after 20 days, and then you need a break and you can understand how long it will last, after learning about it from the doctor. The best result, according to doctors, can be achieved at the expense of low doses, since side effects develop much less frequently, and the effectiveness of the treatment increases.
In laboratory conditions, in time for experiments on rats, it was found that with a concentration of the drug Stefaglabrin sulfate of 0.1-1 mg / kg, the treatment is faster than without it. The course of therapy ended earlier, when compared with animals that did not take this medicine. After 2-3 months, the nerve fibers in the rodents were almost completely restored, and the impulse was transmitted along the nerve without delay. In experimental subjects who were treated without this medication, recovery lasted about six months and not all nerve endings returned to normal.
Copaxone

There is no cure for multiple sclerosis, but there are drugs that can reduce the effect of the immune system on the myelin sheath, and Copaxone is one of them. The essence of autoimmune diseases is that the immune system destroys the myelin located on the nerve fibers. Because of this, the conductivity of impulses worsens, and Copaxone is able to change the goal of the body's defense system to itself. Nerve fibers remain intact, but if the cells of the body have already taken up the erosion of the myelin sheath, then the drug will be able to push them back. This phenomenon occurs due to the fact that the drug is very similar in structure to myelin, so the immune system switches its attention to it.
The drug is able not only to take on the attack of the body's defense system, but also produces special cells of the immune system to reduce the intensity of the disease, which are called Th2-lymphocytes. The mechanism of their influence and formation has not yet been properly studied, but there are various theories. There is an opinion among experts that dendritic cells of the epidermis are involved in the synthesis of Th2-lymphocytes.
The developed suppressor (mutated) lymphocytes, getting into the blood, quickly penetrate into the part of the nervous system where the focus of inflammation is located. Here, Th2 lymphocytes, due to the influence of myelin, produce cytokines, that is, anti-inflammatory molecules. They begin to gradually relieve inflammation in this part of the brain, thereby improving the sensitivity of nerve endings.
The benefit of the drug is not only for the treatment of the disease itself, but also for the nerve cells themselves, since Copaxone is a neuroprotector. The protective effect is manifested in the stimulation of the growth of brain cells and the improvement of lipid metabolism. The myelin sheath mainly consists of lipids, and in many pathological processes associated with damage to nerve fibers, their oxidation occurs, so myelin is damaged. The drug Copaxone is able to eliminate this problem, as it increases the body's natural antioxidant (uric acid). Due to what the level of uric acid rises is not known, but this fact has been proven in the course of numerous experiments.
The drug serves to protect nerve cells and reduce the severity and frequency of exacerbations. It can be combined with medicines Stefaglabrin sulfate and Milgamma.
The myelin sheath will begin to recover due to the increased growth of Schwann cells, and Milgamma will improve intracellular metabolism and enhance the effect of both drugs. It is strictly forbidden to use them on their own or change the dosage on their own.
Is it possible to restore nerve cells and how long it will take only a specialist can answer, focusing on the results of the examination. It is forbidden to take any drugs on your own to improve the sensitivity of tissues, since most of them have a hormonal basis, which means they are difficult to tolerate by the body.
NERVE FIBERS
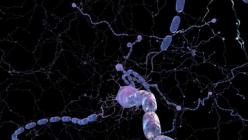
Nerve fibers are processes of neurons covered with glial sheaths. There are two types of nerve fibers - unmyelinated and myelinated. Both types consist of a centrally lying process of a neuron (an axial cylinder) surrounded by a sheath of oligodendroglia cells (in the PNS they are called lemmocytes or Schwann cells).
unmyelinated nerve fibers in an adult, they are located mainly in the autonomic nervous system and are characterized by a relatively low speed of nerve impulse conduction (0.5-2 m/s). They are formed by immersing the axial cylinder (axon) into the cytoplasm of lemmocytes, which are located in the form of strands. In this case, the plasmolemma of the lemmocyte bends, surrounding the axon, and forms a duplication - the mesaxon (Fig. 14-7). Often in the cytoplasm of one lemmocyte there can be up to 10-20 axle cylinders. Such a fiber resembles an electrical cable and is therefore called a cable-type fiber. The surface of the fiber is covered with a basement membrane. In the CNS, especially in the course of its development, unmyelinated fibers are described, consisting of a "naked" axon, devoid of a sheath of lemmocytes.
Rice. 14-7. Formation of myelinated (1-3) and unmyelinated (4) nerve fibers in the peripheral nervous system. The nerve fiber is formed by immersing the axon (A) of the nerve cell into the cytoplasm of the lemmocyte (LC). When a myelin fiber is formed, a duplication of the LC plasmolemma - mesaxon (MA) - is wound around A, forming turns of the myelin sheath (MO). In the myelin-free fiber shown in the figure, several A are immersed in the cytoplasm of the LC (cable-type fiber). I am the core of the LC.

myelinated nerve fibers found in the CNS and PNS and are characterized by a high speed of nerve impulse conduction (5-120 m/s). Myelinated fibers are usually thicker than unmyelinated ones and contain larger diameter axial cylinders. In the myelin fiber, the axial cylinder is directly surrounded by a special myelin sheath, around which there is a thin layer that includes the cytoplasm and the nucleus of the lemmocyte - the neurolemma (Fig. 14-8 and 14-9). Outside, the fiber is also covered with a basement membrane. The myelin sheath contains high concentrations of lipids and is intensely stained with osmic acid, having the appearance of a homogeneous layer under a light microscope, but under an electron microscope it is found that it arises as a result of the fusion of numerous (up to 300) membrane coils (plates).
Rice. 14-8. The structure of the myelinated nerve fiber. Myelin fiber consists of an axial cylinder, or axon (A), directly surrounded by a myelin sheath (MO) and a neurolemma (NL), including the cytoplasm (CL) and lemmocyte nucleus (NL). Outside, the fiber is covered with a basement membrane (BM). The areas of MO, in which the gaps between the myelin turns are preserved, filled with CL and therefore not stained with osmium, have the form of myelin notches (MN).
Myelin sheath formation occurs during the interaction of the axial cylinder and oligodendroglia cells with some differences in the PNS and CNS.
Myelin sheath formation in the PNS : the immersion of the axial cylinder into the lemmocyte is accompanied by the formation of a long mesaxon, which begins to rotate around the axon, forming the first loosely arranged turns of the myelin sheath (see Fig. 14-7). As the number of turns (plates) increases in the process of myelin maturation, they are arranged more and more densely and partially merge; the gaps between them, filled with the cytoplasm of the lemmocyte, are preserved only in separate areas that are not stained with osmium - myelin notches (Schmidt-Lanterman). During the formation of the myelin sheath, the cytoplasm and the nucleus of the lemmocyte are pushed to the periphery of the fiber, forming the neurolemma. The myelin sheath has a discontinuous course along the length of the fiber.

Rice. 14-9. Ultrastructural organization of the myelinated nerve fiber. Around the axon (A) there are coils of the myelin sheath (MMO), externally covered with a neurolemma, and which includes the cytoplasm (CL) and the nucleus of the lemmocyte (NL). The fiber is surrounded on the outside by a basement membrane (BM). CL, in addition to the neurolemma, forms an inner sheet (IL) directly adjacent to A (located between it and the SMO), it is also contained in the zone corresponding to the border of neighboring lemmocytes - the nodal interception (NC), where the myelin sheath is absent, and in areas of loose WMO stacking - myelin notches (MN).
Nodal interceptions (Ranvier)- areas in the region of the border of neighboring lemmocytes, in which the myelin sheath is absent, and the axon is covered only by interdigitating processes of neighboring lemmocytes (see Fig. 14-9). Nodal interceptions are repeated along the course of the myelin fiber with an interval equal, on average, to 1-2 mm. In the region of the nodal node, the axon often expands, and its plasmolemma contains numerous sodium channels (which are absent outside the nodes under the myelin sheath).
Propagation of depolarization in myelin fiber carried out in jumps from interception to interception (saltatory). Depolarization in the region of one nodal junction is accompanied by its rapid passive propagation along the axon to the next junction (since current leakage in the internodal region is minimal due to the high insulating properties of myelin). In the area of the next intercept, the impulse causes the existing ion channels to turn on and a new area of local depolarization appears, etc.
Myelin sheath formation in the CNS: the axial cylinder does not sink into the cytoplasm of the oligodendrocyte, but is covered by its flat process, which subsequently rotates around it, losing the cytoplasm, and its coils turn into plates of the myelin sheath

elbows (Fig. 14-10). In contrast to Schwann cells, one CNS oligodendrocyte with its processes can participate in the myelination of many (up to 40-50) nerve fibers. The axon sites in the area of nodes of Ranvier in the CNS are not covered by the cytoplasm of oligodendrocytes.
Rice. 14-10. The formation of myelin fibers by oligodendrocytes in the CNS. 1 - the axon (A) of the neuron is covered by a flat process (PO) of the oligodendrocyte (ODC), the coils of which turn into plates of the myelin sheath (MO). 2 - one ODC with its processes can participate in the myelination of many A. Areas A in the area of nodal intercepts (NC) are not covered by the cytoplasm of ODC.
Violation of the formation and damage of formed myelin underlie a number of serious diseases of the nervous system. Myelin in the CNS may be a target for autoimmune damage T-lymphocytes and macrophages with its destruction (demyelinization). This process actively proceeds in multiple sclerosis, a serious disease of an unclear (probably viral) nature, associated with a disorder of various functions, the development of paralysis, and loss of sensitivity. The nature of neurological disorders is determined by the topography and size of the damaged areas. With some metabolic disorders, there are disorders in the formation of myelin - leukodystrophy, manifested in childhood by severe lesions of the nervous system.
Classification of nerve fibers
Classification of nerve fibers is based on differences in their structure and function (velocity of nerve impulses). There are three main types of nerve fibers:
1. Type A fibers - thick, myelinated, with far-distant nodal intercepts. Conduct impulses at high speed
(15-120 m/s); subdivided into 4 subtypes (α, β, γ, δ) with decreasing diameter and speed of impulse conduction.
2. Type B fibers - medium thickness, myelin, smaller diameter,
than type A fibers, with a thinner myelin sheath and a lower speed of nerve impulse conduction (5-15 m/s).
3. Type C fibers - thin, unmyelinated, conduct impulses at a relatively low speed(0.5-2 m/s).
Regeneration of nerve fibers in the PNS includes a naturally unfolding complex sequence of processes during which the neuron process actively interacts with glial cells. The actual regeneration of the fibers follows a series of reactive changes caused by their damage.
Reactive changes in the nerve fiber after its transection. During the 1st week after cutting the nerve fiber, ascending degeneration of the proximal (closest to the body of the neuron) part of the axon develops, at the end of which an extension (retraction flask) is formed. The myelin sheath in the area of damage disintegrates, the body of the neuron swells, the nucleus shifts to the periphery, the chromatophilic substance dissolves (Fig. 14-11).
In the distal part of the fiber, after its transection, descending degeneration is noted with complete destruction of the axon, myelin breakdown, and subsequent phagocytosis of detritus by macrophages and glia.
Structural transformations during the regeneration of the nerve fiber. After 4-6 weeks. the structure and function of the neuron are restored, thin branches (growth cones) begin to grow from the retraction flask in the direction of the distal part of the fiber. Schwann cells in the proximal part of the fiber proliferate, forming ribbons (Büngner) parallel to the course of the fiber. In the distal part of the fiber, Schwann cells also persist and mitotically divide, forming ribbons that connect with similar formations in the proximal part.
The regenerating axon grows in the distal direction at a rate of 3-4 mm/day. along the Büngner tapes, which play a supporting and guiding role; Schwann cells form a new myelin sheath. Collaterals and axon terminals are restored within a few months.

Rice. 14-11. Regeneration of the myelinated nerve fiber (according to R.Krstic, 1985, with changes). 1 - after transection of the nerve fiber, the proximal part of the axon (A) undergoes ascending degeneration, the myelin sheath (MO) in the area of damage disintegrates, the perikaryon (PC) of the neuron swells, the nucleus shifts to the periphery, the chromatophilic substance (CS) disintegrates (2). The distal part associated with the innervated organ (in the given example, the skeletal muscle) undergoes downward degeneration with complete destruction of A, disintegration of MO and phagocytosis of detritus by macrophages (MF) and glia. Lemmocytes (LC) persist and mitotically divide, forming strands - Büngner's ribbons (LB), connecting with similar formations in the proximal part of the fiber (thin arrows). After 4-6 weeks, the structure and function of the neuron are restored, thin branches grow distally from the proximal part A (bold arrow), growing along the LB (3). As a result of regeneration of the nerve fiber, the connection with the target organ (muscle) is restored and its atrophy caused by impaired innervation regresses (4). In the event of an obstruction (P) on the path of regenerating A (for example, a connective tissue scar), the components of the nerve fiber
form a traumatic neuroma (TN), which consists of growing branches A and LC (5).
regeneration conditions are: no damage to the body of the neuron, a small distance between the parts of the nerve fiber, the absence of connective tissue that can fill the gap between the parts of the fiber. When an obstruction occurs on the path of the regenerating axon, a traumatic (amputation) neuroma is formed, which consists of a growing axon and Schwann cells soldered into the connective tissue.
There is no regeneration of nerve fibers in the CNS : although CNS neurons have the ability to restore their processes, this does not happen, apparently due to the adverse influence of the microenvironment. After damage to a neuron, microglia, astrocytes, and hematogenous macrophages phagocytize detritus in the area of the destroyed fiber, and proliferating astrocytes form a dense glial scar in its place.
NERVE ENDINGS
Nerve endings- terminal devices of nerve fibers. According to their function, they are divided into three groups:
1) interneuronal contacts (synapses)- provide a functional connection between neurons;
2) efferent (effector) endings- transmit signals from the nervous system to the executive organs (muscles, glands), are present on axons;
3) receptor (sensitive) endingsperceive irritations from the external and internal environment, are present on the dendrites.
INTERNEURONAL CONTACTS (SYNAPSE)
Interneuronal contacts (synapses) divided into electrical and chemical.
electrical synapses rare in the CNS of mammals; they have the structure of gap junctions, in which the membranes of synaptically connected cells (pre- and postsynaptic) are separated by a 2-nm-wide gap pierced by connexons. The latter are tubes formed by protein molecules and serve as water channels through which small molecules and ions can be transported from one cell to another.

another (see chapter 3). When an action potential propagating across the membrane of one cell reaches the gap junction, an electrical current passively flows through the gap from one cell to another. The impulse is capable of being transmitted in both directions and with virtually no delay.
Chemical synapses- the most common type in mammals. Their action is based on the conversion of an electrical signal into a chemical signal, which is then converted back into an electrical signal. The chemical synapse consists of three components: the presynaptic part, the postsynaptic part, and the synaptic cleft (Fig. 14-12). The presynaptic part contains a (neuro)transmitter, which, under the influence of a nerve impulse, is released into the synaptic cleft and, binding to receptors in the postsynaptic part, causes changes in the ion permeability of its membrane, which leads to its depolarization (in excitatory synapses) or hyperpolarization (in inhibitory synapses). ). Chemical synapses differ from electrical synapses in one-sided conduction of impulses, a delay in their transmission (a synaptic delay of 0.2–0.5 ms), and the provision of both excitation and inhibition of the postsynaptic neuron.
Rice. 14-12. The structure of a chemical synapse. The presynaptic part (PRSP) has the form of a terminal button (CB) and includes: synaptic vesicles (SP), mitochondria (MTX), neurotubules (NT), neurofilaments (NF), presynaptic membrane (PRSM) with presynaptic compaction (PRSU). The postsynaptic part (PSCH) includes the postsynaptic membrane (POSM) with the postsynaptic compaction (POSU). The synaptic cleft (SC) contains intrasynaptic filaments (ISF).
1. presynaptic part is formed by the axon along its course (passing synapse) or is an extended end part of the axon (terminal bud). It contains mitochondria, aER, neurofilaments, neurotubules and synaptic vesicles with a diameter of 20-65 nm, which contain the neurotransmitter. The shape and nature of the contents of the vesicles depend on the neurotransmitters in them. Round light vesicles usually contain acetylcholine, vesicles with a compact dense center - norepinephrine, large dense vesicles with a light submembrane rim - peptides. Neurotransmitters are produced in the body of the neuron and are transported to the axon endings by the mechanism of rapid transport, where they are deposited. Partially, synaptic vesicles are formed in the synapse itself by splitting off from the cisterns of the aER. On the inner side of the plasmolemma, facing the synaptic cleft (presynaptic membrane), there is a presynaptic seal formed by a fibrillar hexagonal protein network, the cells of which contribute to a uniform distribution of synaptic vesicles over the surface of the membrane.
2. postsynaptic part It is represented by a postsynaptic membrane containing special complexes of integral proteins - synaptic receptors that bind to a neurotransmitter. The membrane is thickened due to the accumulation of dense filamentous protein material under it (postsynaptic compaction). Depending on whether the postsynaptic part of the interneuronal synapse is the dendrite, the body of the neuron, or (less often) its axon, synapses are divided into axo-dendritic, axosomatic and axo-axonal, respectively.
3. synaptic cleft 20-30 nm wide sometimes contains transverse glycoprotein intrasynaptic filaments 5 nm thick, which are elements of a specialized glycocalyx that provide adhesive bonds of the pre- and postsynatic parts, as well as directed diffusion of the mediator.
The mechanism of transmission of a nerve impulse in a chemical synapse. Under the influence of a nerve impulse, voltage-dependent calcium channels of the presynaptic membrane are activated; Sa 2+ rushes to the axon, the membranes of synaptic vesicles in the presence of Ca2+ merge with the presynaptic membrane, and their content (mediator) is released into the synaptic cleft by the mechanism of exocytosis. By acting on the receptors of the postsynaptic membrane, the mediator causes either its depolarization, the emergence of a postsynaptic action potential and the formation of a nerve impulse, or its hyperpigmentation.
polarization, causing an inhibitory response. Excitatory mediators, for example, are acetylcholine and glutamate, while inhibition is mediated by GABA and glycine.
After the termination of the interaction of the mediator with the receptors of the postsynaptic membrane, most of its endocytosis is captured by the presynaptic part, the smaller part is scattered in space and captured by the surrounding glial cells. Some mediators (for example, acetylcholine) are broken down by enzymes into components that are then captured by the presynaptic part. Synaptic vesicle membranes embedded in the presynaptic membrane are further incorporated into endocytic lined vesicles and reused to form new synaptic vesicles.
In the absence of a nerve impulse, the presynaptic part releases individual small portions of the mediator, causing spontaneous miniature potentials in the postsynaptic membrane.
EFFERENT (EFFECTOR) NERVE ENDINGS
Efferent (effector) nerve endings Depending on the nature of the innervated organ, they are divided into motor and secretory. Motor endings are found in striated and smooth muscles, secretory - in the glands.
Neuromuscular ending (neuromuscular junction, motor plaque) - the motor ending of the axon of the motor neuron on the fibers of the striated somatic muscles - consists of the terminal branching of the axon, which forms the presynaptic part, a specialized area on the muscle fiber, corresponding to the postsynaptic part, and the synaptic cleft separating them (Fig. 14-13).
In large muscles that develop significant strength, one axon, branching, innervates a large number (hundreds and thousands) of muscle fibers. On the contrary, in small muscles that perform fine movements (for example, the external muscles of the eye), each fiber or a small group of them is innervated by a separate axon. One motor neuron, together with the muscle fibers innervated by it, forms a motor unit.
presynaptic part. Near the muscle fiber, the axon loses its myelin sheath and gives rise to several branches that
Multiple sclerosis is another evidence of the imperfection of our immune system, which sometimes “goes crazy” and begins to attack not an external “enemy”, but the tissues of its own body. In this disease, cells of the immune system destroy the myelin sheath of nerve fibers, which is formed during the development of the body from a certain type of glial cells - "service" cells of the nervous system. The myelin sheath covers axons - long processes of a neuron that act as "wires" through which a nerve impulse travels. The sheath itself serves as electrical insulation, and as a result of its destruction, the passage of an impulse along the nerve fiber slows down by 5-10 times.
In the photo, accumulations of macrophages (brown color) are visible along the periphery of the plaques. Macrophages are attracted to the lesion and activated by other cells of the immune system - T-lymphocytes. Activated macrophages phagocytize ("eat") dying myelin, and, in addition, they themselves contribute to its damage, producing proteases, pro-inflammatory molecules, and reactive oxygen species. (Immunohistochemistry, macrophage marker - CD68).
Normally, cells of the immune system, like other blood cells, are not able to penetrate directly into the nervous tissue - they are not allowed by the so-called blood-brain barrier. But with multiple sclerosis, this barrier becomes passable: “crazy” lymphocytes gain access to neurons and their axons, where they begin to attack myelin molecules, which are a complex multilayer protein-lipid structure. This sets off a cascade of molecular events leading to the destruction of myelin and sometimes the axons themselves.
The destruction of myelin is accompanied by the development of inflammation and sclerosis of the affected area, i.e. the formation of a connective tissue scar in the form of a plaque that replaces the myelin sheath. Accordingly, in this area, the conductive function of the axon is impaired. The plaques are located diffusely, scattered throughout the nervous system. It is with this arrangement of lesions that the very name of the disease is associated - “multiple” sclerosis, which has nothing to do with ordinary absent-mindedness (the one that we sometimes talk about in everyday life - “I have completely sclerosis, I forgot everything again”).
The symptoms of multiple sclerosis vary and depend on which nerves are affected. Among them are paralysis, balance problems, cognitive impairment, changes in the functioning of the sense organs (in a quarter of patients, the development of the disease begins with visual impairment due to optic neuritis).
Modern treatment of multiple sclerosis leaves much to be desired.
There is no effective treatment yet, especially since the causes of this disease are still not known, there are only data on the possible influence of the environment and genetic predisposition. For treatment, in addition to symptomatic therapy, which can relieve pain and reduce muscle spasms, glucocorticoid preparations are used to reduce inflammation, as well as immunomodulators and immunosuppressants aimed at suppressing the "bad" activity of the immune system. All these remedies can slow down the development of the disease and reduce the frequency of exacerbations, but do not cure the patient completely. There are no drugs that can repair already damaged myelin.
However, such a drug, aimed specifically at restoring myelin, and not just at slowing down the pathological process, may soon appear. The development under the working title Anti-LINGO-1 from the Swiss company Biogen, the largest manufacturer of drugs for the treatment of multiple sclerosis, is currently undergoing phase 2 clinical trials. The drug is a monoclonal antibody that can specifically bind to the LINGO-1 protein, which prevents the process of myelination and the formation of new axons. Accordingly, if this protein is "turned off", myelin begins to recover.
In animal experiments, the use of the new drug led to 90 percent remyelination. Patients with multiple sclerosis taking Anti-LINGO-1 currently have an improvement in optic nerve conduction. However, the full results of clinical trials on patients will be received only by 2016.