Homeopathic teaching about diseases differs significantly from the classical one. For each homeopathic physician, fixing changes in the patient's condition during therapy is of decisive importance.
Classification of diseases
Diseases can be conditionally divided into acute and chronic. In fact, they differ in their origin, prognosis and method of treatment. Also, both acute and chronic diseases are divided into fixed (the same symptoms and dynamics) and non-fixed (individual symptoms), which makes them different in terms of treatment. Chronic diseases cannot be overcome by the body, they only increase in the course of a person's life. Hahnemann divided them into three main chronic diseases, three miasms: psora (itchy miasm), sycosis (gonorrhea) and syphilis (peptic ulcer).
Conservative treatments
In addition, the development of depression in people with a medical condition has been associated with adverse physical outcomes and a significant increase in disability. Patients suffering from depression after cerebrovascular arrhythmia have been found to have an increased risk of death and a significantly lower effect on measures Everyday life. The clinical course of heart disease is also affected by depression, and 9 out of 10 studies found an increase in cardiovascular mortality among depressed patients.
Acute diseases
Hahnemann describes an acute illness as a rapid process that either has to be cured in a relatively short time or results in death.
Acute illnesses are infections with specific pathogens that either cause permanent immunity for life (eg, rubella) or are capable of recurring (eg, scarlet fever). These include epidemics, infections (observed with a low standard of living, due to lack of nutrition), trauma and acute mental reactions to stress.
Chronic illness and depression: what are the symptoms?
It is not clear to what extent detection and treatment of depression can improve outcome in such cases. The process of diagnosis is often complex, as is the treatment. Antidepressants may aggravate the patient's condition, there is potential for drug interactions, and the presence of impaired renal, hepatic, or gastrointestinal function may alter drug metabolism. Thus, a careful assessment of the risks and benefits is required when choosing an antidepressant. However, antidepressants are effective in people who are medically ill, and antidepressants are tolerated by up to 80% of cancer patients without side effects.
Acute diseases in homeopathy cannot become chronic, as is commonly believed in allopathic medicine. If the disease becomes chronic or recurs, it means that the disease was chronic from the very beginning. And acute childhood illnesses can indicate which chronic diseases the patient is currently active.
Chronic illness superimposed on mental illness
Optimal management of depression in patients with chronic conditions also involves the use of a combination of cognitive and supportive psychotherapy that includes awareness of the grief and loss that are consequences of the disease process. The development of a chronic illness in patients with pre-existing mental illness can exacerbate their symptoms and cause deterioration in their functioning. There may be delays in disease diagnosis in patients with chronic psychotic conditions because these patients may not prioritize their symptoms or they may lack the ability to report their symptoms.
- Fixed acute illnesses
Fixed acute diseases are epidemic diseases with similar symptoms and course. Initially, the symptoms characteristic of such diseases were collected and analyzed, as a result of which the drugs most similar in their actions were selected. Among these drugs, in each individual case, one is selected that suits a particular patient with such a disease according to individual manifestations. Fixed acute diseases include: rubella, scarlet fever, chicken pox, measles, viral or bacterial infectious diseases.
Osteomed and chronic diseases of internal organs
Ethical issues may arise when considering the ability of such patients to accept or decline treatment. Psychiatrists play a valuable role in helping patients understand the medical problems they face and assess their ability to make informed decisions.
Physical Consequences mental illness deserve attention in their own right. After an episode of major depression, the risk of myocardial infarction increases 4-5 times when other medical factors are controlled. Depression in women is associated with a decrease in bone density. Thus, depressive episodes may contribute to the development medical conditions that are chronic.
It is worth saying that in the case of acute surgical diseases and injuries, homeopathic therapy is secondary. Primarily it is necessary to stop the bleeding, bandage the wound, etc.
- Unrecorded acute illnesses
Unfixed acute diseases are characterized by individual symptoms. In such cases, it is necessary to understand whether intervention is really necessary or the body can cope on its own. The choice of a homeopathic remedy is determined by a combination of characteristic acute symptoms, as well as the cause of the disease. The choice of a homeopathic remedy is determined by a combination of characteristic acute symptoms or a cause. If a chronic disease was treated with a homeopathic remedy before the onset of acute symptoms, it is necessary to wait a little before taking action, as this may be an exacerbation or manifestation of some old symptom.
Physical symptoms as an expression of emotional dysfunction
The development of new symptoms in a previously stable patient may indicate that the patient is emotionally distressed. Aggravation of established illness, such as the development of pseudo-epidemics in a patient with epilepsy, may indicate adjustment difficulties, depression, or difficult social problems or relationship problems. The key symptoms of so-called somatoform disorders are physical complaints, excessive fear of physical illness, or excessive and unreasonable desire for medical or surgical treatment.
- Diagnosis and therapy of acute diseases
Acute diseases include such conditions as, for example, a significant increase in temperature, childhood illnesses, epidemics, gastroenteritis. With a simple course of the disease, as a rule, acute conditions do not require intervention, but in the case of a complicated course of the disease, the use of the drug is required as soon as possible. Most often, a single dose of a homeopathic remedy is required. At the same time, a slight deterioration at the very beginning immediately after taking the remedy must be waited out. In the case of an obvious improvement, but without a final recovery, the patient needs to take a second dose of the drug. With a change in symptoms, the manifested symptoms are subject to analysis and new repertorization. The newly prescribed drug will lead the healing process further. If the condition worsens significantly, one should not wait, it is necessary to repertorize and select a new remedy. Also, after taking a drug that is characteristic of the patient's acute condition, he may need to take a constitutional remedy in order to level the residual symptoms of the acute illness.
Despite their frequency in general medical practice, these problems can be among the most challenging for physicians, and physicians report finding patients with these disorders among the most challenging. The use of effective communication methods by the physician can reduce the risk of chronic morbidity and disability.
Patients with chronic diseases may provoke feelings of anxiety and inadequacy of professionalism; they can also become an emotional burden for the physician, who is subjected to the cumulative suffering and loss experienced by patients and their families. Countering these feelings can be the satisfaction that comes from providing consistent and unwavering care and deep appreciation expressed by patients.
chronic diseases
In classical medicine, the concept of chronic disease refers to a disease that lasts more than three months or recurs more than three or four times. Thus, an acute illness can become chronic. In homeopathy, however, this is impossible, since initially any disease is either acute or chronic. The maximum that can happen is if the homeopathic doctor treats the disease as acute, but it is essentially chronic.
Maintaining patient hope
For patients and their families, hope is an essential part of coping. The clinician plays a key role in creating real hope. However, healthy coincidence differs from the popular notion of “positive thinking.” It involves the ability to tolerate and express concerns and emotions, not just the ability to delay worry. The ability to discuss the anxieties, uncertainties and fears, loss and sadness that usually accompany severe illness is generally helpful, despite the pressure usually placed on the patient by family and friends to always "keep a positive attitude." appearance». « positive thinking", may represent an attempt to avoid a distress chronic diseases and the physicians who care for these patients and their families are not immune to these forms of coping.
A sign of a chronic disease in homeopathy is the inability of the body to heal itself, and therefore the disease gradually progresses, leading to death. Chronic diseases are manifested by persistent symptoms, or progress in jerks that outwardly resemble an acute disease. Chronic diseases are often hereditary, presenting with symptoms from birth or throughout life. Also, chronic diseases can be acquired. Acquired chronic diseases differ from congenital ones in the characteristic stages of their course. In congenital chronic diseases, there are no stages during the course.
A study of women with breast cancer found that those who sought alternative therapies had higher rates of psychological morbidity: thus seeking such treatments may be indicative of a patient's distress rather than their well-being.
Transition to the terminal phase
Recognizing that the condition has progressed and that the patient is approaching the terminal phase of their illness can be frustrating for staff who knew the patient well. In some cases, the patient may be reluctant to discuss the need to change treatment goals or the possibility of death, but in other cases it is the doctor's avoidance that limits the likelihood that the patient has raised these issues. Employees may be reluctant to give up their more aggressive treatments. It should be remembered that medical professionals evaluate the treatments they take differently from the assessments made by cancer patients.
Hahnemann described three chronic diseases - psora (itchy miasm), sycosis (gonorrheal miasm) and syphilis (chancre miasm). Allen J. added to this list another chronic acquired disease, which is called pseudopsora (tuberculin miasm). Laborde and Rich also added the cancer miasm to the list.
In the case of a chronic disease, it is extremely important to take a detailed history in order to distinguish this disease from the visible manifestations of an acute ailment, as well as in order to understand the cause and recognize the pathogen. Besides, great importance have in this case the constitution of the patient, his biography and family history.
Chronically ill patients sometimes report surprisingly high levels of satisfaction with their quality of life. In addition, clinicians may underestimate the quality of life of patients with chronic diseases and elderly patients. Patients may place more importance on their mental health than their physicians; physicians can focus on their patients' "physical limitations".
Treatment side effects of treatment
Side effects of some treatments, such as those caused by steroids, can lead to frustration and anger; these feelings may be mediated by the emotional response to changes in the patient's body and symptoms, but may also be a direct result of the treatment's effect on the patient's mood. The doctor may feel guilty about these side effects. In addition, patients who become angry, demanding, or resentful can generate a strong sense of anger in the staff.
Fixed chronic diseases
In cases of chronic diseases, Hahnemann gave similar recommendations as in the case of fixed acute diseases.
Unfixed chronic diseases
Chronic diseases that have become chronic are treated in the same way as non-fixed acute diseases according to the law of beating.
Although adherence to the prescribed treatments may improve the course of the disease, the physician cannot promise the patient that "being good" will be rewarded; in some diseases, such as diabetes, the disorder may still occur. Young patients, in particular, may test limitations and challenge the status and knowledge of caregivers. Compliance may be poor even in organ transplant patients. There may be conflict between the patient and the clinician about the proposed treatment.
In chronic fatigue syndrome, for example, evidence has emerged about the benefits of cognitive therapy and the importance of exercise. If patients and families are resistant to these approaches, long-term care may be adversely affected. Psychosocial interventions are increasingly being incorporated into routine health care and these approaches appear to be effective. In patients with rheumatoid arthritis, the use of stress management interventions resulted in significant improvements in measures of helplessness, dependence, coping, and pain.
In otolaryngology, throat diseases are considered the most frequently diagnosed pathologies. This applies to children and adult patients. Most cases of acute diseases are recorded in the winter season, however, in some cases, the process becomes chronic, and therefore the symptoms are almost constant.
Relatively simple interventions that allow patients with asthma and rheumatoid arthritis to express the psychological impact of their disease and other stressors have significantly improved symptoms in these patients. Families of patients who are chronically ill tend to be more depressed and more prone to other psychological symptoms. Clinicians should be aware of this hidden morbidity among caregivers.
Recognition of the cost of care
Clinicians who treat patients with chronic disease should not ignore their own needs. Clinicians can be overwhelmed by the emotional needs of their patients. When the clinical course is turbulent or the patient refuses treatment or commits suicide, the sense of professional isolation and despair can be intense. There is strong socialization against members of the medical profession who discuss their problems for fear of being weak. At least half of the physicians in one study reported high levels of emotional exhaustion.
Tonsillitis will be called chronic if there is an inflammatory process in the tonsils, and symptoms appear from time to time. Under the influence of some provoking factors, an exacerbation of the pathology occurs, which is accompanied by an increase in the intensity of symptoms.
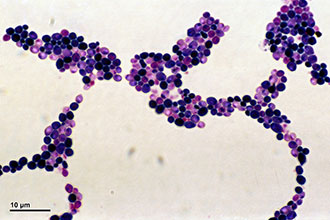
The palatine and other tonsils perform a protective function, as they are lymphoid structures and part of the immune system. Frequent attacks of pathogenic microorganisms against the background of weakened immunity lead to the development of acute tonsillitis, followed by a transition to a chronic form.
The opposite of feelings of helplessness and the limited availability of affordable treatments can elicit a range of responses from healthcare professionals. These responses may include rejection and abandonment of the patient, blaming the patient for the failure to recover, or excessive personal responsibility for the patient's failure to recover. Both under- and over-treatment of the patient may occur. in the widespread debate about caring for dying patients and physicians responding to "incurable" suffering.
The risk of developing a chronic type of the disease increases with a decrease in the body's resistance after infectious diseases (measles, influenza, scarlet fever), with hypothermia or exacerbation of chronic diseases.
Especially often the chronic form is recorded when the infection spreads from foci in the nasopharynx (sinusitis) or oral cavity (caries).
Health professionals do not work in a vacuum. For example, the technological complexity of medical treatment in areas such as transplant surgery and intensive care leads to physicians facing complex ethical issues related to service extensions or resource allocation. There is a requirement for "evidence-based care", but in many areas evidence is either not available or limited, which raises additional concerns among clinicians.
Methods of treatment of chronic tonsillitis
The responses of healthcare professionals to complex clinical situations depend on their training and life experience. The clinical experience of junior physicians, rotating in a variety of specialties and participating in specialist training programs, often does not give them experience in treating patients over a long period. Short-term contact with patients with severe chronic diseases in a hospital setting can provide junior physicians with a distorted view of the course of such diseases, the role of medical treatment, the needs of patients, and their own potential responses.
In addition, chronicity is observed with improper treatment of an acute process, when inadequate antibiotic therapy is prescribed.
The prescription of antibiotics should be carried out exclusively by a doctor based on the results of an antibiogram.
Predisposing factors include:
- violation of nasal breathing with polyposis, adenoids, anomalies of the structure and curvature of the septum;
- inadequate oral hygiene;
- incorrectly selected bracket systems.
ENT diseases of the throat with lesions of the tonsils are classified into:

Symptomatically chronic diseases are not manifested by pronounced signs. A person may be disturbed by perspiration, scratching in the throat, the presence of a lump in the oropharynx, dryness and an unpleasant odor. After each exacerbation of tonsillitis, the improvement in the condition occurs extremely slowly, accompanied by the preservation of subfebrile condition and malaise.
Exacerbations with a simple form are recorded up to three times a year, and in the case of toxic-allergic - much more often, predisposing to the formation of a paratonsillar abscess and the spread of inflammation to neighboring healthy tissues (laryngitis). The patient complains of subfebrile hyperthermia and constant weakness.
With a chronic disease of the throat, the tonsils become a focus of infection, from which microbes spread throughout the body. Consequently:
- reduced immune defense;
- collagenoses are noted (dermatomyositis, periarteritis, lupus, scleroderma);
- skin diseases develop (eczema, dermatitis, psoriasis);
- nerve endings are affected (sciatica);
- autoimmune processes develop (vasculitis, thrombocytopenic purpura);
Diagnosis of a throat disease includes the collection of anamnestic information (), an examination by an otolaryngologist and additional studies.
With pharyngoscopy, when the throat is examined, the disease is manifested by redness of the mucous membrane, thickening, and swelling of the arches. In children, loosening of the tissue of the tonsils is often found. Purulent discharge with an unpleasant odor accumulates in the lacunae. Palpation of the regional lymph nodes reveals lymphadenitis (enlargement, swelling, soreness of the lymph nodes).
Among the pathologies of the upper respiratory tract, pharyngitis is considered the most common. Previously, the acute process ended in recovery and did not lead to complications. Nowadays, more and more patients turn to the otolaryngologist with chronic diseases. In this case, the larynx is exposed to prolonged exposure to an infectious agent, which predisposes the preservation of inflammation.
When throat disease is suspected, the chronic stage can take several forms:
- catarrhal, which is characterized by an unexpressed clinical picture;
- hypertrophic, which is characterized by the growth of the mucosa and ridges;
- atrophic, when atrophy of the mucous membrane of the posterior pharyngeal wall occurs, which significantly disrupts its function.
Sometimes there is a mixed form, in which some parts of the larynx are hypertrophied, while others have undergone atrophy, which is manifested by fuzzy symptoms.
The causes that provoke the chronicity of the pathological process include viral pathogens (parainfluenza, adenoviruses, rhinoviruses) that persist for a long time in the mucosa. With frequent infectious lesions, the immune defense is so reduced that it cannot resist infection with streptococci or staphylococci.
As a result, even the slightest hypothermia or cold drinks can provoke an exacerbation of the disease. The disease becomes chronic against the background of:

It is worth noting that chronic inflammation is possible with gastroesophageal reflux disease, when food is thrown, irritating the mucous membrane.
Allocate a consistent change in the mucosa, ranging from catarrhal symptoms, ending with atrophy.
The catarrhal form is often observed in smokers, as well as with the negative action of professional factors. With the multiplication of microbes and the release of toxic substances, swelling and redness of the tissues are observed. A plaque of dead cells and pathogenic microorganisms can form on the surface.
In the future, there are large accumulations of mucus on the mucosa, which is difficult to cough up. The granulosa stage is considered the most dangerous in terms of the spread of infection.
| stages | Symptoms | Picture with pharyngoscopy |
|---|---|---|
| catarrhal | Discomfort, dryness, tickling, itching in the oropharynx, soreness when swallowing, sensation of a lump | Not pronounced hyperemia of the posterior pharyngeal wall, slight thickening, swelling of the mucosa, the presence of thick mucus, which becomes more liquid during exacerbation. In some cases, the tongue and arches become edematous and hyperemic. |
| granulosa | Vomiting, burning, severe cough. | Red nodules (granules) are visualized on the walls, plugs appear in the tonsils, the trigeminal nerve is irritated by granular accumulations, and follicles also increase. |
| Hypertrophic | Discomfort, sensation of a lump, difficulty swallowing, mucus dripping from the nasopharynx, frequent dry cough, unpleasant odor. | Purulent mucus is located on the edematous, hyperemic walls, the walls of the larynx, the lateral ridges of the arch are compacted. Purulent secretions can form crusts, and the granules gradually increase, provoking a transition to the atrophic stage. |
| atrophic | Dryness, perspiration in the oropharynx, sensation of a lump, the presence of crusts, cough, pain when swallowing. | Sclerotic changes in the mucosa and submucosa of the pharyngeal wall and lymphoid structures. Thick mucus with a purulent component accumulates, forming dense crusts. The walls become thinned, pale, lacquered, through which fragile vessels are visualized. |
At the hypertrophic stage, tissue thickening is observed. With atrophy of the mucosa, crusts form, which can be released when coughing. Lymph nodes are also enlarged and painful on palpation.
The disease in children passes in a catarrhal form, without causing clinical symptoms without exacerbation.
In adults, the disease manifests itself:
- unexpressed perspiration;
- viscous secretions of small volume;
- the presence of a lump in the oropharynx;
- nausea, vomiting when coughing;
- dryness, irritation of the mucous membrane when inhaling cold air;
- rare cough;
- regional lymphadenitis;
- increased manifestations in the morning.
Complications are represented by the spread of inflammation to the surrounding organs with the development of tracheitis, bronchitis or otitis media. In adults, there is a risk of transition of the catarrhal form to hypertrophic and atrophic, disrupting the function of the pharynx. Concomitant damage to the Eustachian tube leads to a decrease in auditory function.
The diagnosis uses the analysis of anamnestic information, pharyngoscopy, laryngoscopy and laboratory tests (blood test, smears).
 The formation of an inflammatory focus caused by a fungal infection is called pharyngomycosis. IN Lately otolaryngologists note the growth of fungal infection of the oropharynx. In most cases, pharyngomycosis is combined with stomatitis, gingivitis or cheilitis.
The formation of an inflammatory focus caused by a fungal infection is called pharyngomycosis. IN Lately otolaryngologists note the growth of fungal infection of the oropharynx. In most cases, pharyngomycosis is combined with stomatitis, gingivitis or cheilitis.
It should be noted that fungal infection is much more severe than bacterial inflammation and is less amenable to therapy. The cause of the development of the disease can be:
- yeast-like fungi candida, causing thrush, candidiasis of the skin and genitals;
- mold fungi (5%).
Activation and reproduction of a fungal infection is noted against the background of immunodeficiency in HIV, frequent colds, tuberculosis, or severe concomitant pathology (hypothyroidism, diabetes). In addition, the wrong course of antibiotic therapy, which exceeds the recommended dosages and duration, should be attributed to predisposing factors. Also, pharyngomycosis is promoted by prolonged use of hormonal, chemotherapeutic drugs and removable dentures.
There are several forms of the disease:
- pseudomembranous, with a white coating on the surface of the oropharynx;
- erythematous, characterized by hyperemic areas with a smooth, varnished mucosal surface;
- hyperplastic - manifested by the formation of whitish plaques, which are difficult to separate from the mucous membrane, leaving a bleeding wound;
- erosive-ulcerative, when ulceration affects only the surface layers.
Sympathetically, the disease is manifested by uncomfortable sensations in the form of perspiration, burning, dryness and tickling in the oropharynx. Soreness is not very pronounced, increases with food intake, especially pickles and spices.
Pain may radiate to the ear and neck area. Lymphadenitis and deterioration of the general condition (fever, severe malaise, cephalgia, dizziness) are also observed.
The chronic course of pharyngomycosis is characterized by exacerbations more than 10 times a year. Chronization contributes to improper treatment of the acute stage. There is also a risk of pharyngeal, paratonsillar abscess and fungal sepsis, which leads to the occurrence of infectious foci in the internal organs.
In diagnosis, it is important to study in detail the anamnestic data (previous course of antibacterial, hormonal, immunosuppressive drugs).
With pharyngoscopy, edema and films on the mucosa are revealed. Sites of fungal infection are localized on the tonsils and the posterior pharyngeal wall with a possible spread to the tongue, larynx and esophagus. When affected by Candida fungi, the raids have a whitish tint, curdled character and are easily removed from the surface. Mucous at the same time hyperemic, areas with ulceration.
If mold fungi became the cause of pharyngomycosis, yellowish films are removed with difficulty, leaving a bleeding surface. In differential diagnosis, pathology should be distinguished from diphtheria. Also, pharyngoscopy reveals uneven reddening of the mucosa, thickening of the ridges against the background of atrophic changes, and vessels are visualized.
Laboratory analysis (microscopy and culture method) is considered decisive in the diagnosis. The study of smears makes it possible to confirm the fungal origin of the disease and to establish the sensitivity of pathogenic microorganisms to drugs.
Among benign neoplasms with localization in the throat, it is worth highlighting adenoma, fibroma, papilloma, cystic formations, lipoma and teratoma. Predisposing factors include smoking, alcohol abuse, dust inhalation, poor hygiene, as well as chronic infectious and inflammatory diseases of the oropharynx and nasopharynx.
Of the clinical symptoms, it should be noted:

The diagnosis is established on the basis of clinical signs and examination of the oropharynx during pharyngoscopy. To assess the prevalence of the oncoprocess, rhinoscopy, otoscopy, radiography, computed and magnetic resonance imaging are prescribed. A biopsy is performed to determine the cellular composition of the tumor.
Differential diagnosis is carried out between malignant tumors, scleroma and Hodgkin's disease.
throat cancer
According to the cellular composition of malignant tumors, carcinoma, lymphoepithelioma, cytoblastoma, and reticucytoma are distinguished. Tumors are characterized by rapid growth and metastasis, when malignant foci form in distant organs.
The difficulties of early detection of pathological neoplasms in the throat are due to the absence of clinical signs at the initial stage.
With progression, the disease is manifested by a sensation of a foreign element in the oropharynx, choking, difficulty swallowing and pain. Numbness of some parts of the pharynx is also possible.
In addition to local symptoms, general manifestations are observed. These include cephalgia, severe malaise, decreased appetite, weight loss, fatigue, and pale skin. When the malignant process spreads to blood vessels bleeding is possible. Hearing may also decrease - with damage to the Eustachian tube, which leads to the development of chronic otitis media.
The defeat of the nasopharynx predisposes to the appearance of an inflammatory process in the paranasal sinuses (sinusitis). If the tumor is injured by solid food or undergoes decay in stages 3, 4, the risk of an unpleasant odor and blood in the saliva increases.
Diagnosis includes analysis of anamnestic data, physical examination, pharyngoscopy and histological analysis. To detect metastases, radiography, endoscopic, ultrasound techniques, as well as computed and magnetic resonance imaging are prescribed.
What are the diseases of the throat, we have analyzed. Finally, it should be noted that the correct treatment of an acute pathological process prevents the development of a chronic course of the disease.



